Intrauterine insemination (IUI)
- What is it?
- After sexual intercourse, sperm has to travel from the vagina to the uterus and then to the woman’s fallopian tubes, where it could fertilize an egg. The goal of IUI is to insert sperm directly into the woman’s uterus, bringing it as close to the egg as possible. Ovarian stimulation is often added to the procedure to increase the success rate.
- Ovarian stimulation is used to cause the ovaries to produce more than one egg.
- Medications that can be used for ovarian stimulation:
- Clomiphene citrate
- Letrozole
- Human menopausal gonadotropin (hMG)
- Follicle-stimulating hormone (FSH)
- After sexual intercourse, sperm has to travel from the vagina to the uterus and then to the woman’s fallopian tubes, where it could fertilize an egg. The goal of IUI is to insert sperm directly into the woman’s uterus, bringing it as close to the egg as possible. Ovarian stimulation is often added to the procedure to increase the success rate.
WHAT ARE THE CHANCES OF PREGNANCY PER IUI CYCLE?
- 10-14% when using injectable medications: human menopausal gonadotropin (hMG) or follicle-stimulating hormone (FSH).
- These chances hold for the first 3-4 attempts, after which they decline.
- Chances will be lower if the female partner is older (advanced maternal age is defined as 35 years or older) or if she doesn’t have many eggs left.
- Success rates are also dependent on the cause of infertility.
- Pros
- Not as invasive or expensive as IVF.
- This treatment has few side effects when used without ovarian stimulation.
- Cons
- With or without stimulation the woman may experience discomfort during and/or after the procedure.
- The ovarian stimulation medication can cause:
- Ovarian hyperstimulation syndrome (swollen and painful ovaries, accumulation of fluid in abdomen and chest).
- Women sometimes report mood swings or feeling overly emotional while taking the hormones needed for stimulation.
- Ovarian stimulation along with IUI carries a greater risk of having a multiple birth. This increases the risk of pregnancy, such as having babies who are born too early and/or low birthweight.
In vitro fertilization (IVF)
- What is it?
- During IVF, eggs are taken from the ovaries and combined with sperm inside a dish, outside the woman’s body. In fact, In Vitro is actually Latin for In glass. The embryo that results from this combination is then transferred back into the uterus.
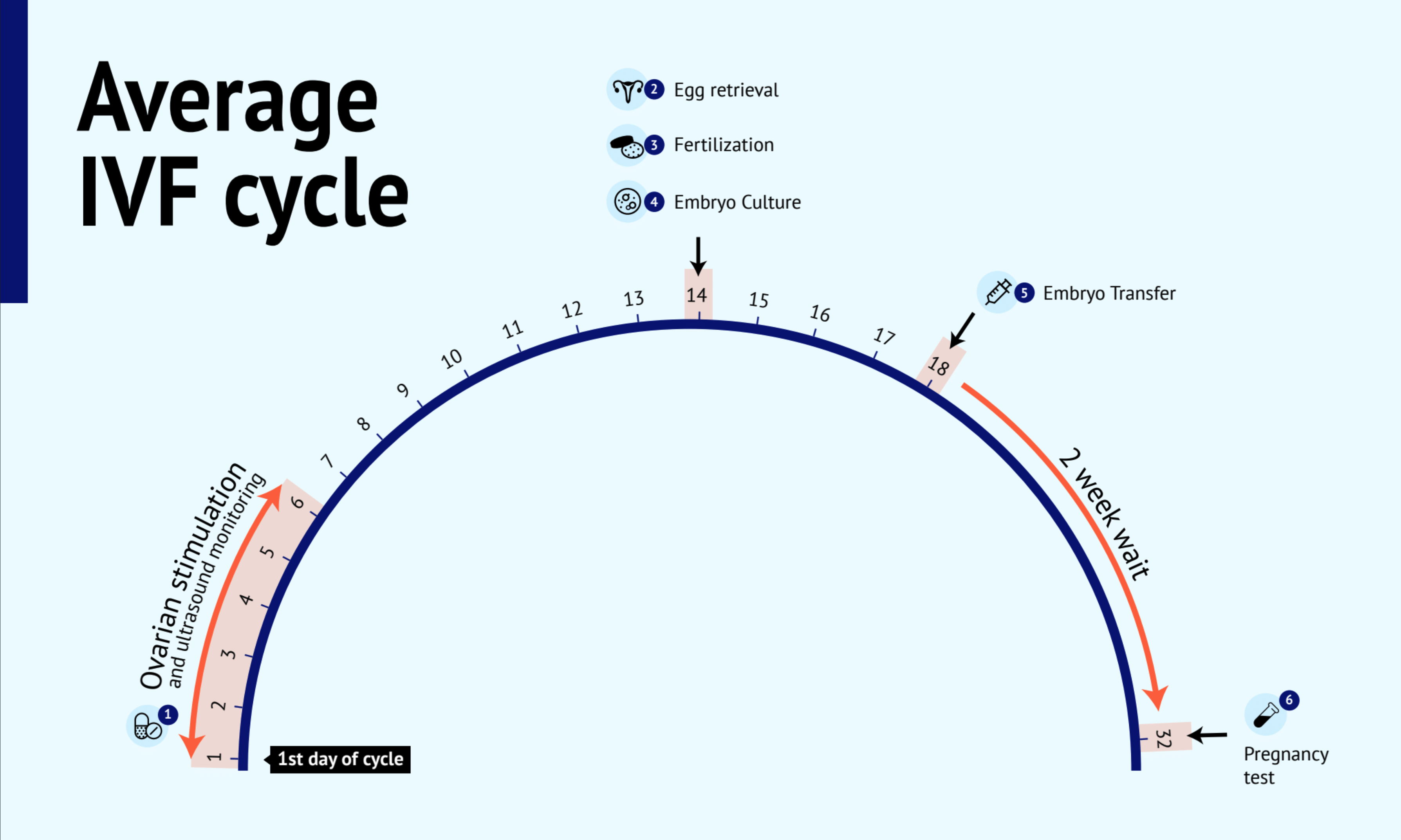
Step 1: Ovarian stimulation & ultrasound monitoring
What is it?
- Ovarian stimulation is used to cause the ovaries to produce more than one egg.
Medications that can be used for ovarian stimulation:
- Clomiphene citrate
- Letrozole
- Human menopausal gonadotropin (hMG)
- Follicle-stimulating hormone (FSH)
Ultrasound monitoring
- Your partner will need to go to the fertility clinic for an ultrasound approximately every two days for monitoring, so your doctor can see how your partner’s egg follicles are growing, and occasionally for a blood test.
Step 2: Egg retrieval
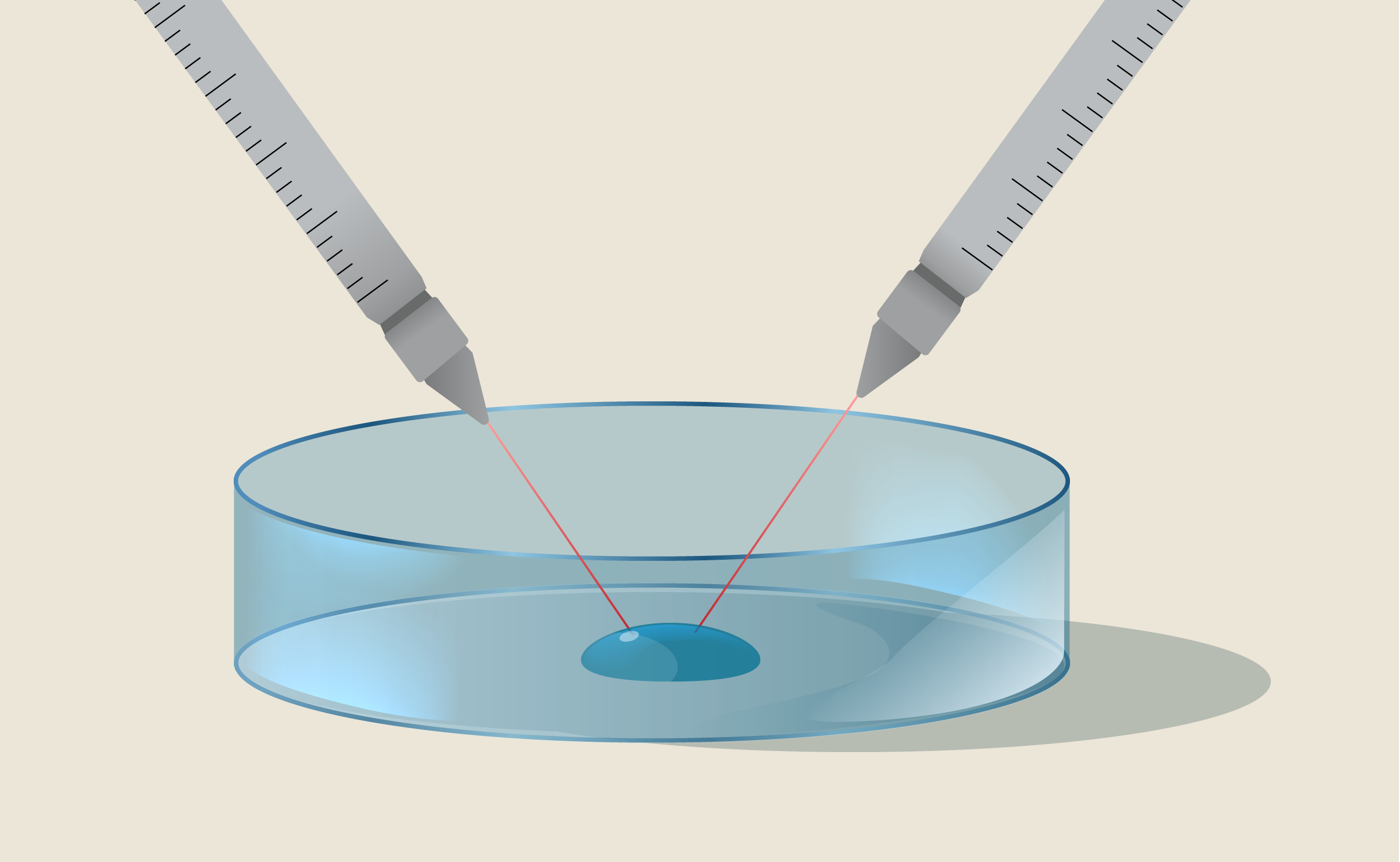
- Egg retrieval is the process of removing eggs from the woman’s ovary. This procedure is done under the guidance of an ultrasound, meaning that the doctor will insert a wand in the vagina to look inside the woman’s uterus and guide the procedure.
- Using a fine needle that is carefully inserted through the vagina, the doctor will identify the egg follicles produced through stimulation. Then, the doctor will drain the fluid inside the egg follicles and retrieve the egg. This is done for every follicle that contains an egg. Women are sedated during the procedure to reduce the pain.
Step 3: Fertilization
- Once eggs are retrieved, they will need to be fertilized.
- Depending on you and your partner’s condition, you may be advised to do standard IVF or ICSI.
- Standard IVF allows the sperm and egg to come together “naturally” in a dish.
- ICSI (intracytoplasmic sperm injection) is the process of injecting a sperm into each mature egg. It is commonly used when sperm are either low in quality, quantity, or have high DNA fragmentation. This can also be done if a small number of eggs were retrieved.
- This can help increase the chances of the egg being fertilized, but it does not necessarily increase the chances of pregnancy or delivering a healthy baby.
Step 4: Embryo cultures
- The fertilized eggs or embryos are grown in incubators over the next few days in dishes containing special food for embryos called “culture media.”
- The embryos are cultured for 3 to 5 days before they are transferred to the uterus or frozen for future use.
- The embryos can be tested in some IVF centres to screen for genetic abnormalities before they are transferred into the uterus (preimplantation genetic testing).
Step 5: Embryo transfer
- Depending on the woman’s age, the quality of the embryos, and other factors, one or more embryos are transferred into the uterus. An ultrasound is used to make sure that the embryo is placed in the right location.
- If there are extra embryos remaining, they can be frozen for future use. These frozen embryos can be used for future embryo transfer attempts, without the need to go through ovarian stimulation again.
Step 6: Pregnancy test (b-HCG blood test)
- Approximately 12 days after the embryo transfer, your partner will have a blood test to verify if a pregnancy was achieved. Results are usually available the same day the blood is taken. If the blood test results are positive for pregnancy, your partner will usually repeat the blood test 48 hours later to determine whether the b-HCG levels are rising appropriately.
- What are the chances of pregnancy?
- IVF success rates depend on many factors, such as the egg’s age and quality. In women using their own eggs who are under the age of 35, it can be as high as 50% or more per cycle. Success rates decline in the mid to late 30s, and drop rapidly in the early 40s. By age 44 success rates are lower than 5%.
- A woman’s ovarian reserve also has a significant impact on success rates. The lower the ovarian reserve, the lower the chances of pregnancy.
- Pros
- Has the highest success rate of all fertility treatment options.
- You can choose to perform genetic screening of embryos to decrease the risk of inherited diseases and determine which embryo has the best chance of making a healthy baby.
- Possibility of preserving extra embryos for future cycles.
- The number of embryos transferred can be controlled to minimize the risk of multiple pregnancy.
- Cons
- This is a costly procedure.
- Risk of ovarian hyperstimulation syndrome (OHSS), which results in swollen and painful ovaries and accumulation of fluid in the abdomen and chest.
- Risk of infection and bleeding from egg retrieval.
- Women sometimes report physical symptoms such as bloating, some weight gain, and headaches from ovarian stimulation medication.
- Women sometimes report mood swings or feeling overly emotional while taking the hormones needed for stimulation.
- Increased risk of having a multiple birth if more than one embryo is transferred, which increases the risk of pregnancy.
- There is a very small chance (2%) that the embryo may implant on the fallopian tube rather than in the uterus, leading to an ectopic pregnancy.
Using donor sperm, eggs, or embryos
Due to the risk of genetic disease or problems with sperm and/or eggs, some couples may opt to use a sperm and/or egg donor to conceive.
Donors are people who decide to donate their sperm or eggs. They undergo medical screening to test for conditions such as sexually transmitted infections or genetic diseases. A donor’s frozen sperm can be used for intrauterine insemination or in vitro fertilization. A donor’s eggs can be used fresh or frozen for cycles of in vitro fertilization.
The egg donor undergoes ovarian stimulation and egg retrieval, while the receiver gets medication to prepare her uterus for implantation.
When couples are diagnosed with both male and female factor infertility, donated embryos can be used. These embryos are grown in vitro from donated sperm and eggs.
Risks
Are there risks to our (potential) child, if we conceive?
There is a slight chance that a child born as a result of fertility treatments will be of lower birth weight and/or preterm. This risk depends on your partner’s age, current health status, number of embryos transferred, and treatment type.