Abnormal cervical mucus
- What is it?
- Something is wrong with the mucus that comes out of the vagina, called cervical mucus. This is a problem because cervical mucus helps transport sperm to the egg.
- How common is it?
- Not very common
- Tests and treatment options
- There aren’t really any tests for this problem – the doctor usually makes this diagnosis after ruling out other potential causes.
- A woman with abnormal cervical mucus may be offered:
- Intrauterine insemination (IUI)
- In vitro fertilization (IVF)
Advanced maternal age
- What is it?
- As a woman gets older, her egg quality slowly decreases. After age 35, women are at greater risk of infertility as they may have poor egg quality, (meaning the eggs, once combined with sperm, are less likely to develop into healthy embryos), and they may not have as many eggs as they once had (medical speak: lack of “ovarian reserve”).
- How common is it?
- If a woman is over 35, she is considered to be of “advanced maternal age.”
- Tests and treatment options:
- There’s no way to tell how good a woman’s eggs are (egg quality), but it is possible to tell how many eggs she has left.
- A blood test will likely indicate these two things:
- Low levels of the hormone produced in the follicles, the part of a woman’s ovary that holds the eggs. This hormone is called anti-Mullerian hormone (AMH). If a woman’s level of AMH is low, this indicates that there are few remaining follicles. This blood test can be done at any time during a woman’s cycle.
- The hormone responsible for producing mature eggs, follicle stimulating hormone (FSH), will also be tested around day 3 of a woman’s cycle. High levels of FSH mean that the ovarian reserve is probably low.
- The doctor will probably want to do a vaginal ultrasound, an ultrasound where a probe is placed in the vagina to better see the ovaries.
- Some follicles are visible on the ultrasound. These visible follicles are called antral follicles. The doctor will use the vaginal ultrasound to count the number of follicles, called the antral follicle count (AFC). A low AFC is associated with decreased ovarian reserve.
- There are a variety of treatment options:
- Ovulation induction
- Ovulation induction can be tried with natural intercourse.
- Intrauterine insemination (IUI)
- IUI can be tried with or without ovarian stimulation.
- In vitro fertilization (IVF)
- Egg donation, embryo donation
- Ovulation induction
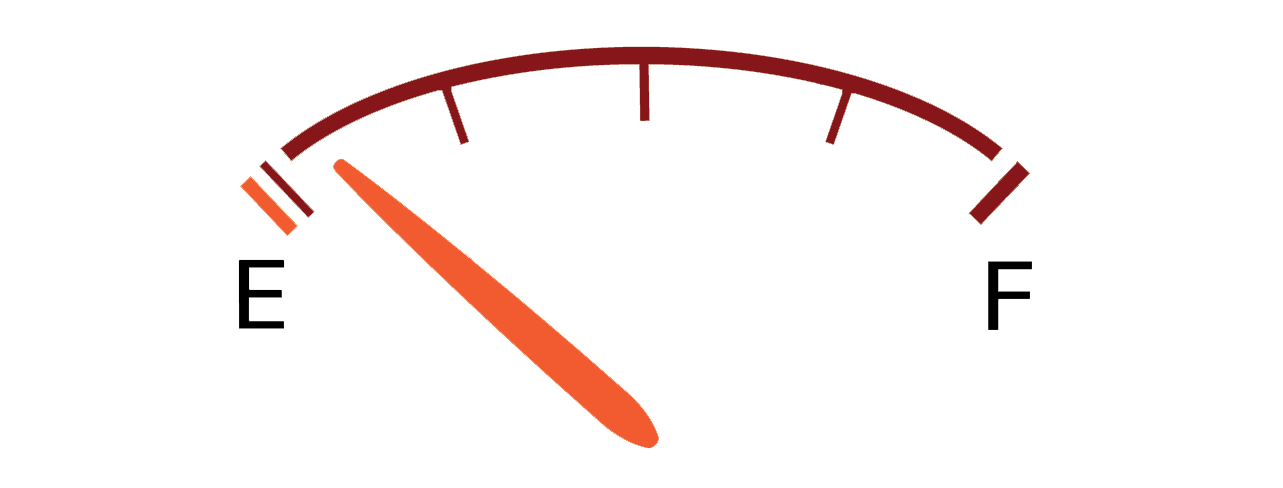
Diminished ovarian reserve
- What is it?
- There are relatively few eggs left in the ovaries, and the ones that are left may be of poor quality.
- How common is it?
- It depends on a woman’s age. In women under the age of 30, it is very uncommon. In women in their late 30s or older, it becomes increasingly common.
- What should she be looking for?
- There are not many symptoms.
- Initially, a woman may experience shorter menstrual cycle lengths, for example, 21 to 24 days instead of 28 to 30. Later, her cycles might become completely unpredictable and irregular as reserves get lower.
- If she’s had previous surgery to her ovaries, chemotherapy or radiation therapy, she may be at higher risk.
- If she has a family history (e.g. her mother went into menopause at an early age).
- Smoking increases the chances.
- Tests and treatment options:
- There’s no way to tell how good a woman’s eggs are in terms of quality, but it is possible to tell how many eggs she has left.
- A blood test will likely indicate these two things:
- Low levels of the hormone produced in the follicles, the part of a woman’s ovary that holds the eggs. This hormone is called anti-Mullerian hormone (AMH). If a woman’s level of AMH is low, this indicates that there are few remaining follicles. This blood test can be done at any time during a woman’s cycle.
- The hormone responsible for producing mature eggs, follicle stimulating hormone (FSH), will also be tested around day three of a woman’s cycle. High levels of FSH mean that the ovarian reserve is probably low.
- The doctor may want to do a vaginal ultrasound, where a probe is placed in the vagina to better see the ovaries.
- Some follicles are visible on the ultrasound. These visible follicles are called antral follicles. The doctor will use the vaginal ultrasound to count the number of follicles, called the antral follicle count (AFC). A low AFC is associated with decreased ovarian reserve.
- There are a variety of treatment options:
- Ovulation induction
- Ovulation induction can be tried with natural intercourse.
- Intrauterine insemination (IUI)
- IUI can be tried with or without ovarian stimulation.
- In vitro fertilization (IVF)
- Egg donation, embryo donation
- Ovulation induction
Endometriosis
- What is it?
- The tissue in a woman’s uterine cavity is present in places it shouldn’t be, like the ovaries.
- How common is it?
- In infertile women, it is common: 30-40% of these women have endometriosis.
- What should she be looking for?
- Some women do not have any symptoms. But, if a woman has really painful periods, pain when she’s having sex, or trouble getting pregnant, these could be some signs that she has endometriosis.
- If other women in her family have endometriosis, she may be at increased risk, as there is some evidence that it is hereditary.
- Tests and treatment options:
- The doctor may perform a pelvic examination to check for anything out of the ordinary.
- The doctor may also perform an ultrasound to determine what may be causing symptoms. Cysts from endometriosis may be detected on ultrasound, but endometriosis isn't always visible.
- To confirm a diagnosis of endometriosis, a woman will have to have surgery. While she is under general anaesthesia, her doctor will perform a laparoscopy involving a biopsy of her uterus. This involves making small cuts (3-4) on her lower abdomen, and inserting a small camera through her bellybutton to look around. The doctor can take a tissue sample (biopsy) and also remove any endometrial tissue that may be found.
- Treatment options:
- Surgery to remove endometrial tissue.
- Ovulation induction
- Ovulation induction can be tried with natural intercourse.
- Intrauterine insemination (IUI)
- IUI can be tried with or without ovarian stimulation.
- In vitro fertilization (IVF)
- Egg donation, embryo donation
Fallopian tubes impaired or blocked
- What is it?
- The tubes that carry a woman’s eggs from the ovaries are blocked. This also means that the sperm can’t travel to her egg.
- How common is it?
- Somewhat common. If only one tube is blocked, a woman may still be able to get pregnant naturally.
- What should she be looking for?
- Many women don’t have any symptoms.
- A previous sexually transmitted infection (STI) that went untreated and/or led to pelvic inflammatory disease (PID) may increase risk.
- Previous pelvic or abdominal surgery, ruptured appendix or bowel
- Inflammatory Bowel Disease
- Endometriosis
- Any woman who has had previous pelvic inflammatory disease (PID), regardless of cause, is also at increased risk.
- Smoking also increases the risk.
- Tests and treatments:
- The doctor may order one of the following tests:
- Sonohysterogram: a special kind of ultrasound that shows the inside of the uterus. A small amount of salt solution (saline) is placed in the uterus with a small tube (catheter). The doctor then performs a transvaginal ultrasound to see if the solution runs into any road blocks. It is generally done at the doctor’s office and takes about 15–20 minutes.
- Hysterosalpingogram: a special kind of X-ray where a dye is placed in the uterus with a small tube (catheter). If there is a blockage, the dye won’t be able to travel throughout her reproductive system.
- If either test shows abnormal results, she may be offered surgery to open up her tubes. Other treatment options include:
- In vitro fertilization (IVF)
- Egg donation, embryo donation
- The doctor may order one of the following tests:
Fibroids
- What are they?
- Fibroids are smooth muscle masses that grow in the uterus. Generally, they’re non-cancerous.
- How common are they?
- Somewhat common: 25% of women have fibroids, but most fibroids do not cause infertility.
- African American women, women who are older (over 35), and women who are obese are at greater risk.
- What should she be looking for?
- Many women don’t notice anything. However, if she feels pain or pressure in her pelvic region, has bleeding not during her period, or if she is having urinary or bowel problems, she may have a fibroid.
- Tests and treatment options:
- The doctor may perform one of the following tests to look for fibroids:
- Ultrasound: A probe is placed into the vagina, to see the uterus, ovaries, and Fallopian tubes.
- MRI: A magnetic resonance image (MRI) will be taken of the uterus. This will require going into a tube where numerous pictures are taken of the insides of a woman’s body. Usually, a salt solution (saline) is used to help doctors locate the fibroids.
- If fibroids are found, they can be removed through surgery (myomectomy) or treated with special fibroid-shrinking drugs (GnRH agonist, ulipristal acetate). The choice of treatment depends on the number, size, and location of the fibroid(s).
- The doctor may perform one of the following tests to look for fibroids:
Polycystic ovarian syndrome
- What is it?
- Polycystic ovarian syndrome (PCOS) is a hormonal condition where a woman’s follicles don't mature and androgen levels are elevated. While the word “cysts” is in the name of this condition, PCOS doesn’t mean that a woman has ovarian cysts. Instead, it’s that she has immature follicles that appear on an ultrasound as a set of pearls on her ovaries.
- How common is it?
- 5–10% of women have PCOS.
- What should she be looking for?
- Persistent irregular menstrual cycles
- Excess facial hair and/or acne throughout lifetime
- Many, but not all, women who have PCOS are also over-weight or obese.
- Tests and treatment options:
- A diagnosis of PCOS will be made if a woman has 2 of the following 3 conditions:
- She reports irregular or no periods.
- A physical examination reveals lots of facial hair and/or acne, or a blood test reveals high levels of androgen hormone.
- An ultrasound reveals 12 or more follicles on either ovary.
- Depending on the severity of the condition, the doctor may recommend:
- Weight loss and exercise
- Medical treatment with insulin-sensitizing medications, like metformin
- Inducing ovulation with medications, such as clomiphene citrate or an aromatase inhibitor like letrozole, or injections of follicle stimulating hormone (FSH)
- Intrauterine insemination (IUI) with ovarian stimulation
- Laparoscopic ovarian drilling: A surgical treatment that can stimulate ovulation. This involves making small cuts in the abdomen (3-4); a camera is then placed inside to look at the follicles. Parts of the ovaries are destroyed during this procedure.
- This is not a procedure that is done frequently.
- It requires the woman to be fully asleep (general anaesthesia is used).
- She can go home after the procedure and there is a recovery time of a few days to 4 weeks.
- In vitro fertilization (IVF)
- A diagnosis of PCOS will be made if a woman has 2 of the following 3 conditions:
Polyps
- What is it?
- Growths in the uterus. They are generally non-cancerous. They are referred to both as uterine polyps and endometrial polyps.
- How common is it?
- 35% of women will have a polyp at some point in their reproductive life.
- What should she be looking for?
- Women who are older (>35), are obese and have previously or are currently taking tamoxifen (a drug used to treat breast cancer), or who have a past risk of polyps are at higher risk of having polyps.
- Sometimes women experience heavier periods, frequent or unpredictable bleeding, and/or bleeding after sex.
- Tests and treatments:
- The doctor will probably want to look and see if she has polyps. Here are some common methods:
- Transvaginal ultrasound - an ultrasound where a probe is placed in the vagina to better see her reproductive organs.
- If a polyp is found, a hysteroscopy that involves removal of the polyp will be performed.
- Sonohysterogram: a special kind of ultrasound that can trace the inside of the uterus. A small amount of salt solution (saline) is placed in the uterus with a small tube (catheter). The doctor then performs a transvaginal ultrasound to see if the solution runs into any road blocks. It is generally done at the doctor’s office and takes about 15–20 minutes.
- If a polyp is found, a hysteroscopy that involves removal of the polyp will be performed.
- Hysteroscopy: A small tube is placed inside the vagina that allows the doctor to look inside the uterus. During this procedure, the doctor may remove any polyps that are found.
- The recovery is about 1–2 days and she may experience some slight bleeding.
- Transvaginal ultrasound - an ultrasound where a probe is placed in the vagina to better see her reproductive organs.
- The doctor will probably want to look and see if she has polyps. Here are some common methods: