Getting pregnant is more complicated than it seems in the movies
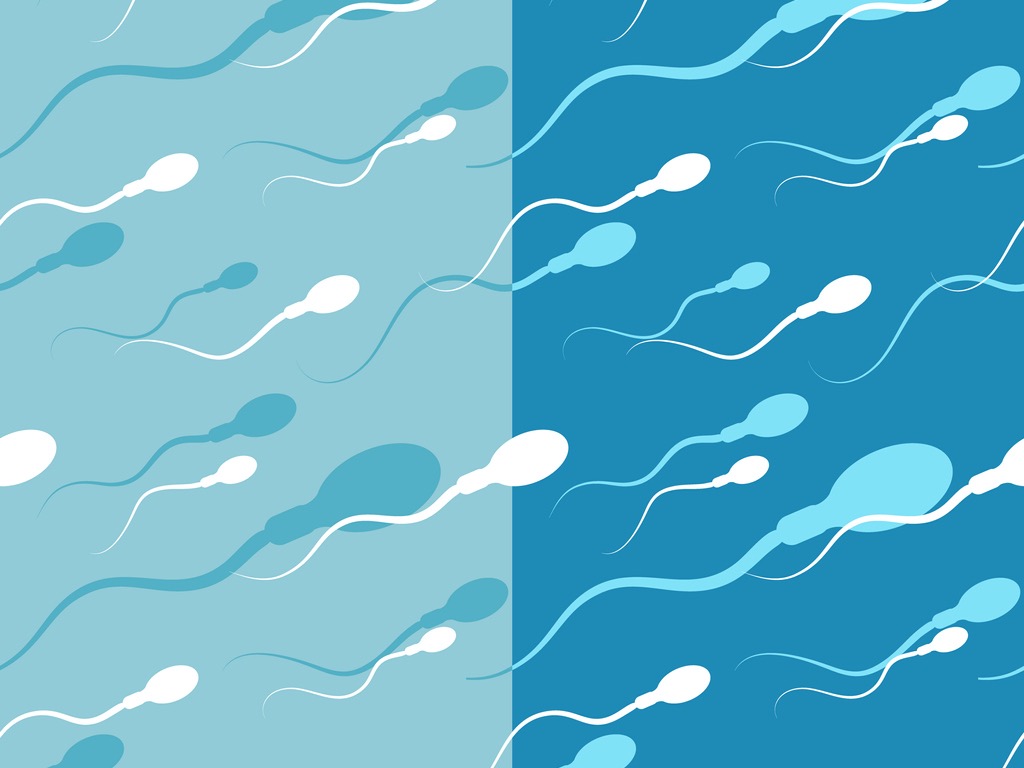
Many things have to be working well. A sperm analysis will tell you whether there are any problems with the movement, shape, or number of sperm. If you are able to provide a sperm sample, that’s the first step in figuring out whether sperm quality or quantity is contributing to your fertility issues.
“So we went through testing, semen analysis all the things that she needed to go through and it kinda came down to the conclusion that it was a low semen count for me that was the issue and so we decided to do whatever was best.” (Fertility patient, 34)
Once you have used the cup to collect your sperm sample, you will give the cup to a nurse or lab technician (depending on the clinic, you may not have to hand your sample to someone in person but instead leave it in a specific spot). Your ejaculate will be analyzed to make sure that there are enough sperm and that they are the right shape and are moving well. Sometimes the clinic will test your sperm’s DNA, a molecule that contains your genetic code, with a DNA fragmentation test. This test checks for breakages in the DNA strands, which can make it more challenging to have a successful pregnancy.
As long as your doctor can find some good quality sperm, they will be able to choose the best ones to use in IVF/ICSI.
Here’s some information about providing a sperm sample and what the test results mean.
There isn’t enough ejaculate
Medical speak: Absent/Low-volume ejaculate
Here are some reasons why you may have had little (less than 1.5 ml) or no sperm in the cup:
I missed the cup (medical speak: Incomplete collection)
Causes and risk factors:
- Having to ejaculate in an unfamiliar environment or under pressure (like at a fertility clinic) may mean that you’re not getting it all in the cup.
Tests and treatments:
- Check out our tips for collection here. Your doctor may advise you to not have sex or masturbate 2–5 days before coming to the clinic.
- Some more tips to make sure it’s all getting in the cup:
- Prepare the cup by removing the lid of the container and make sure it’s close by.
The sperm is going the wrong way (medical speak: Retrograde ejaculation (RE))
Causes and risk factors:
- Your semen is going into your urinary bladder instead of your testes. Diabetes, certain medications (e.g., alpha blockers to treat high blood pressure such as alfuzosin and doxazosin), neurological injuries, or previous surgeries to your urinary bladder or pelvis can cause this.
Tests:
- An analysis of your urine after you have ejaculated (post-ejaculate urinalysis (PEU)). You will have to provide a urine sample after you provide a sperm sample. The urine is then examined for the presence of sperm to confirm retrograde ejaculation (RE). If your urine has sperm in it, your sperm may be going the wrong way, known as retrograde ejaculation.
Treatments:
- Treatment of the underlying health condition (e.g., diabetes)
- Certain medications, such as the over-the-counter decongestant drug Sudafed (Pseudoephedrine) or the prescription drug imipramine
- Sperm can also be collected from the urine and “washed” for use in IUI or IVF.
The sperm can’t get out (medical speak: Obstruction)
Causes and risk factors:
- The ducts where the ejaculate comes out are blocked.
- You have a neurological or metabolic disease, such as diabetes.
- You do not have a vas deferens.
- You’ve had a history of trauma to your genitals.
- You’ve had a procedure done on your urinary tract.
Tests:
- An analysis of your urine after you have ejaculated (post-ejaculate urinalysis (PEU)). You will have to provide a urine sample after you provide a sperm sample. If your sperm can't get out, not only would you not have any sperm found in your semen, even the urine sample after ejaculation may not have any sperm inside.
- You may also have to undergo a transrectal ultrasound (TRUS), which will look for an obstruction by inserting an ultrasound probe into the rectum. If your doctor finds cysts, they can be removed to help unblock the roadway.
Treatments:
- Since your sperm is not coming out, it must be found. Here are some ways your sperm can be located. (Once the physicians find it, they will generally be able to use it in IUI, IVF or IVF/ICSI. Click here to learn more about Assisted Reproductive Technologies).
- Cleaning it out – The ducts where the ejaculate comes out are cleaned out to try to remove the blockage (medical speak: Transurethral resection of ejaculatory duct (TURED)).
- Taking it out and using it for ART:
- Sperm is taken from the part of the body where it hides (medical speak: Percutaneous Epididymal Sperm Aspiration (PESA)).
- Sperm is taken from the testicle (medical speak: Testicular aspiration).
- A small amount of tissue from the testicle is taken to look for sperm (medical speak: Percutaneous testicular sperm extraction).
You’ve misfired (medical speak: Failure of emission)
Causes and risk factors:
- You are able to reach orgasm, but do not ejaculate. This may be caused by a spinal cord injury, neurological disease, metabolic disease such as diabetes, major abdominal surgery, an obstruction, severe hypogonadism (very low testosterone), or medications that affect your ejaculation.
Tests:
- An analysis of your urine after you have ejaculated (post-ejaculate urinalysis (PEU)). You will have to provide a urine sample after you provide a sperm sample. If you have a failure of emission, your analysis will show no sperm in your urine. If the test is positive for sperm, the cause may be that your sperm is going the wrong way, known as retrograde ejaculation (RE).
- A transrectal ultrasound (TRUS) could be performed to look for an obstruction in your reproductive system. This is done by inserting an ultrasound probe into the rectum. If the TRUS is normal, then you are likely to have a problem with emission.
Treatments:
- Medications that stimulate circulation, sympathomimetic medications
- Electroejaculation
- Epididymal or testicular sperm aspiration and ICSI
There isn’t enough sperm
Medical speak: Oligospermia or oligozoospermia (low sperm count).
If there isn’t enough sperm in your semen, it may be due to one of the following reasons:
Post-sperm production problems (medical speak: Post-testicular causes). Post-testicular causes are problems that occur after the sperm is made. Sometimes this means the passageways are blocked.
Symptoms: You may notice or are told that there isn’t much ejaculate coming out (less than 1.5 ml).
Risk factors:
- The ducts where the ejaculate comes out are blocked.
- You have had pelvic injury or have had procedures that involve your urinary tract.
Test and treatments:
- An analysis of your pee (urine) after you have ejaculated (post-ejaculate urinalysis (PEU)). You will have to provide a urine sample after you provide a sperm sample. A post-testicular cause will show no sperm in your urine. If it is positive for sperm, the cause may be that your sperm is going the wrong way, known as retrograde ejaculation (RE).
- A transrectal ultrasound (TRUS) could be performed to look for an obstruction in your reproductive system. This is done by inserting an ultrasound probe into the rectum. If the TRUS is normal, then you are likely to have a blockage that can be corrected through surgery, and sperm can be found to use in IVF/ICSI.
Low hormone levels (medical speak: Androgen deficiency)
Symptoms: If your hormones, including your testosterone levels, are out-of-whack, you’ll probably have noticed the following:
- Low sex drive
- Trouble getting it up, known as “erectile dysfunction”
- Feeling very tired
- Feeling sad (depressed)
- Not having as many muscles as you used to
- Having lower amounts of ejaculate than you’ve previously had
Risk factors:
- Getting older
- An illness that affects your entire body, such as cancer, stroke, or a heart attack
- Obesity
- Injury to your testicles
Tests and treatments:
- A blood test will help determine the amount of testosterone you have. If your testosterone levels are borderline or low to normal, you may have androgen deficiency.
- If you have low testosterone levels, this will most likely be treated with human chorionic gonadotropin (hCG) therapy. This therapy tells the testes to produce testosterone. If it isn’t enough, sometimes testosterone will be added.
Enlarged vein(s) in your scrotum (medical speak: Varicoceles)
15% of all men and about 40% of infertile men have enlarged veins in the scrotums. If you’re looking for enlarged veins, look on the left side first (90% of varicoceles are left-sided).
Tests:
- Physical examination: Pull down your pants. Your doctor will want to get a good look at your scrotum in different positions. The physical examination will also involve touching your scrotum to confirm the presence of the vein. You may also be asked to hold your breath and bear down, or cough (Valsalva maneuver) to help your doctor identify a varicocele.
- If your doctor expects that enlarged veins may be the problem, you may also have to undergo a scrotal ultrasound, which will determine how large that vein really is.
Treatments:
- Enlarged veins do not always require treatment, as they are not dangerous if your general health is good.
- If treatment is indicated because of abnormal semen parameters or pain, there are two surgical options: microsurgical varicocelectomy and varicocele embolization. Both treatment options are equally effective and generally require only localized numbing procedures (local anesthesia). You will be able to get back to work 24 hours after the surgery. More intense activities, such as running, may be restricted for about 2–3 weeks.
- A varicocelectomy is an outpatient surgical procedure that involves tying off the blood flow to the vein that is affected.
- A varicocele embolization is an outpatient, minimally invasive medical procedure that involves placing a tiny coil or fluid into a blood vessel to prevent the blood from refluxing back to the testis.
Testicular cancer
Symptoms:
- You may not experience any symptoms. This is why it is important to do regular testicular self-examinations. If you find a lump on the testicle, see your doctor right away.
- Patients with advanced cancer may have symptoms such as abdominal/back pain or shortness of breath.
Risk factors:
- Undescended testis
- Family history of testicular cancer
- Personal history (If you have had cancer in one testicle, you have a higher risk of developing cancer in the other testicle.)
Tests and treatments:
- If a lump is discovered on examination, a scrotal ultrasound should be performed.
- If confirmed, initial workup should include semen analysis and blood tests (medical speak: tumor markers).
- If you are diagnosed with testicular cancer, you may need to have a surgery to remove the testis with cancer. As the surgery and other cancer treatments may affect your fertility, it is best to preserve your sperm right away before your surgery and other cancer treatments. This can be done at your fertility clinic.
Things around you that can affect your hormones and fertility (medical speak: Gonadotoxin exposure)
Symptoms: You probably won’t experience any symptoms.
Risk factors:
- nicotine or tobacco use
- excessive alcohol use
- marijuana use
- chemotherapy, such as methotrexate
- radiation therapy
- pesticide exposure
- heavy metal exposure
Tests and treatments: Reducing your exposure to these environmental risks can change the status (quantity and quality) of your sperm.
No reason, there just aren’t enough sperm
Sometimes after all the poking and prodding, your doctor will tell you there just aren’t enough sperm. In this case, maybe you’ll want to change your diet, engage in some exercise or try some alternative treatments such as acupuncture. Your doctors may suggest more treatments such as medications and surgeries.
There isn’t any sperm present in the ejaculate
Medical speak: Azoospermia
If you don’t have any sperm in that cup, it is often due to one of the following factors:
Pre-sperm production problems (medical speak: Pretesticular causes)
Pretesticular causes are generally associated with too little hormones, known as hypogonadotropic hypogonadism, which may be due to:
- Kallmann syndrome
- Pituitary tumor
- Steroids/testosterone use
Symptoms:
- You may not notice any symptoms. However, if your testosterone is low, you may feel tired and weak. You could also experience a lack of sex drive or the inability to "get it up". If you have a problem with your pituitary gland (the part of your brain that controls hormone production), you may experience headaches and/or visual disturbances.
Tests and treatments:
- Physical examination: Your doctor will do an examination to make sure that you have all your parts and that they’re the right size. The doctor is looking to make sure you have your vas deferens, and also to check out your testicular size and whether you have enlarged veins in your scrotum. Men with pretesticular hormonal problems, secondary hypogonadism, can have small testes.
- Blood test: Your blood will be tested for hormone levels.
- A low level of follicle stimulating hormone (FSH), the hormone that helps with sperm production, may indicate that you have hypogonadotropic hypogonadism.
- A CT Scan or an MRI is often done to look at your pituitary gland. If there is a problem with your pituitary gland, it generally can be treated with medication or surgery.
Problems with sperm production (medical speak: Primary testicular failure)
Symptoms:
- You probably won’t have any symptoms. If you’ve noticed that you have smaller testicles compared to other men, there could be a problem.
Risk factors:
- Problems with your genes (e.g., Klinefelter Syndrome), history of infections (e.g., mumps, chlamydia), injuries and "twisting" of the testes (testicular torsion), history of chemotherapy or surgery.
Tests:
- Physical examination: Your doctor will do an examination to make sure that you have all your parts and that they’re the right size. The doctor is looking to make sure you have your vas deferens, and also to check out your testicular size. Small testicular size can be due to primary (testicular) or secondary (pretesticular) hypogonadism.
- Blood test to check hormones, including the hormone that is in charge of sperm production, follicle stimulating hormone (FSH)
- High FSH suggests primary testicular failure.
- Genetic tests:
- You will be given a blood test to ensure that your chromosomes are okay.
Treatment options:
- If the problem is hormonal, you may be given some medication to help balance your hormones.
- The physician may advise you to try a surgery called microTESE to attempt retrieving sperm for IVF/ICSI. Click here to read our article on microTESE and other sperm retrieval techniques.
There is something blocking the sperm from getting out (medical speak: Post-testicular (obstructive) causes)
Symptoms: You generally won’t have any symptoms.
Risk factors:
- You don’t have a vas deferens.
- The tube that carries the sperm from the testicles to the penis is blocked (medical speak: vasal obstruction).
- You’ve had a vasectomy.
- The epididymis is blocked (medical speak: epididymal obstruction).
Tests and treatments:
- Physical examination: Your doctor will do an examination to make sure that you have all your parts and that they’re the right size. The doctor is looking to make sure you have your vas deferens, and also to check out your testicular size. You’ll probably have normal size testicles, but may not have a vas deferens.
- If you do not have the vas deferens, this is often due to a mutation of the cystic fibrosis gene (CFTR gene), which can be confirmed with a blood test. Absence of the vas deferens means that sperm are still produced by the testes, but they do not come out during ejaculation to get into the semen. Sperm can still be retrieved by doing a biopsy of the testicles (TESE) or by one of the commonly used sperm retrieval techniques: percutaneous epididymal sperm aspiration (PESA), microsurgical epididymal aspiration (MESA), or testicular sperm aspiration (TESA).
- If there is a blockage leading to the vas deferens, known as an epididymal obstruction, sometimes surgery can help (medical speak: vasoepididymostomy).
- If the cause of the blockage is a previous vasectomy, this can often be reversed through surgery (medical speak: vasovasostomy).
- Blood tests:
- The hormone that regulates sperm production, the follicle stimulating hormone (FSH), is measured and is usually normal. If it is not normal, you probably do not have a blockage and may have a hormonal condition.
- Blood tests can also be done to confirm the presence or absence of the cystic fibrosis gene (CFTR).
Sperm aren’t swimming well
Medical speak: Asthenospermia or asthenozoospermia (sperm present but poor motility)
You probably won’t be able to notice that you have sperm that aren’t swimming well. Here are some common causes of asthenospermia:
Your body is fighting your own sperm (medical speak: Anti-sperm antibodies (ASA))
Symptoms: You may not have any symptoms.
Risk factors:
- You’ve previously had surgery in your scrotum (medical speak: prior scrotal surgery).
- Your scrotum has been injured in some way (medical speak: scrotal trauma).
- You have had testicular cancer.
- You have a large vein in your scrotum (medical speak: varicocele vein).
- You have an infection somewhere down there, or you have had a previously untreated infection.
Tests and treatments:
- Your doctor can order a special anti-sperm antibody test to see if your body is fighting sperm.
- If this test is positive for anti-sperm antibodies, a special wash can be applied to the ejaculate to get rid of the antibodies.
- The sperm may then be used for IUI or IVF.
- A short-term course of corticosteroids (e.g., prednisone) may be used to decrease antibodies.
- If this test is positive for anti-sperm antibodies, a special wash can be applied to the ejaculate to get rid of the antibodies.
Prolonged abstinence
Symptoms: You likely won’t feel anything
Recommendations:
- Have sex or masturbate more frequently. You should have sex or masturbate every 2 to 5 days to maintain high sperm quality.
There’s a problem with your testicles
Symptoms: You likely won’t experience any symptoms.
Risk factors:
- Your sperm analysis shows that some sperm have unusual shapes (medical speak: sperm structural defects).
- You have a sexually transmitted infection (STI).
- You have a genital tract infection.
- You have large veins in your scrotum (medical speak: varicocele vein).
- Your testicles are hot:
- This can be caused by being overweight or obese, riding a bike, placing a laptop on your lap, fever, long use of hot bath or sauna, wearing tight briefs, or sitting too long.
Tests and treatments:
- Your doctor can order a test to make sure that you don’t have anything that is fighting your sperm (anti-sperm antibody test).
- If the test is normal, there is probably another cause.
- If a semen analysis shows slow sperm motility, then problems such as varicocele, heat exposure, and infection should be investigated.
- A semen culture may be done to see if there is an infection.
- If it isn’t due to an infection, try to cool off those testicles by wearing loose clothes, placing your laptop on a desk or tray and taking frequent standing breaks during the day.
- If a semen analysis shows that your sperm are not moving, your doctor may also order another test called a viability assay.
- This test can help narrow down the problem. If the test shows that most sperm are alive (medical speak: viability is high), your sperm may be weirdly shaped.
- In addition to semen analysis, additional tests to evaluate the quality of your sperm may be ordered by your doctor. The results of these tests may help your doctor assess if the sperm can be used for IUI or IVF/ICSI.
There is a problem between your testicles and your penis
Symptoms:
- You may or may not have noticed that you have little ejaculate (less than 1.5 ml).
Risk factors:
- Part of the ducts that carry the sperm are blocked (medical speak: partial ductal obstruction).
- You may have previously had pelvic injury or procedures performed on your kidneys, bladder or ureters (urological procedures).
Treatment options:
- If the test that checks if your immune system fights your sperm (medical speak: anti-sperm antibody test) is normal, there may be another cause for your sperm’s lack of swimming technique.
- If the motility of your sperm is very low (less than 5%), a test called a viability assay can help determine if there are live (viable) sperm.
- If most of your sperm are dead (medical speak: low viability), you may have a partial blockage in the ducts where you ejaculate. This can be confirmed with a transrectal ultrasound (TRUS), and treated surgically or worked around with the use of IVF/ICSI.
- A TRUS is done by inserting an ultrasound probe into the rectum.
- If most of your sperm are dead (medical speak: low viability), you may have a partial blockage in the ducts where you ejaculate. This can be confirmed with a transrectal ultrasound (TRUS), and treated surgically or worked around with the use of IVF/ICSI.
Your sperm just can’t swim
- Sometimes doctors find no cause and your sperm are just bad swimmers.
- Your doctor may recommend that you and your partner try IVF/ICSI to get pregnant.
There's not enough sperm and they aren't high quality
Medical speak: Oligoasthenoteratospermia or oligoasthenoteratozoospermia (OAT)
This means a combination of low sperm count, poor sperm movement, and abnormal sperm shape.
Symptoms:
- You may notice that you have a large vein in your scrotum. This is known as a varicocele vein. You generally won’t have any other symptoms, but if you do, the most common one is scrotal pain. You may also notice that the testicle with the varicocele is smaller.
Causes and risk factors:
- Genetics
- Older age
- Use of certain medications (e.g., anabolic steroids)
- Abnormal hormone levels
- Infections of the reproductive system
- Varicocele
- Lifestyle choices (e.g., alcohol consumption, smoking)
- Exposure to some toxic hormones in your environment (medical speak: gonadotoxin exposure), for example through tobacco use, radiation therapy, or contact with pesticides or heavy metals
- Tests and treatments will be offered based on your specific underlying cause(s) and severity of the condition.